Why Does My Back Hurt in Ellicott City MD?

It’s a common but dreaded experience: you wake up with lower back pain in Ellicott City MD. The pain by itself is annoying, but on top of this you are also baffled by the fact that you don’t remember doing anything that could have hurt it. Was it that game of pickleball you played yesterday? You’ve played it plenty of times before and it didn’t seem to be a problem then. But you know that your dad had a disc bulge and he had similar pain…is this genetic? Did you get the short straw in the genetic lottery?
Why Does My Back Hurt?
You make an appointment with your general practitioner and x-ray is ordered (along with a prescription for an anti-inflammatory and a muscle relaxant). You have the x-rays taken. Ah, there’s the problem. Degenerative joint disease, undoubtedly the result of excessive wear and tear on the joints. Wear and tear from what? The gym? Pickleball?
The pain continues. A referral to pain management is made. Epidural steroid injections and physical therapy are ordered. They don’t seem fun, but at least you’re glad to be getting some answers–except that the injections don’t seem to help. Meanwhile the PT told you that your spine is degenerating because your core is weak, but that can’t be right–you do planks and crunches all the time, and the new dead bugs, clamshells, and glute bridge exercises you were prescribed don’t seem to be making a difference either. What happened? The cause of the pain was staring at you right there on your x-ray. Perhaps spinal surgery is necessary. Really? How did this happen? You’re too young for this. A growing sense of fear creeps in, but at the same time something doesn’t feel right. Is this really necessary?
All Too Common
There are many variations of this frustrating and unnerving scenario, some more dramatic than others, but it’s estimated that 85% of adults will experience low back pain at some point in their lifetime. It's one of the top reasons people go to their doctor after upper respiratory infections or colds. In addition, 10 to 40% will experience the associated symptom of sciatica (a general term for pain in the back of the thigh, sometimes extending down to the calf or foot, as a result of irritation to the sciatic nerve). It’s a staggering number, but it should cause us all to ask a question: why is this so common, and what can be done about it?
You Are Not Your MRI in Ellicott City MD
It seems logical, or course. You have lower back pain and an image was ordered and there it is, evidence of degeneration all over the place. Except…spinal degeneration is common, even in those not experiencing low back pain: 37% of 20-year-olds with no symptoms showed evidence of spinal degeneration according to a review of 33 studies; this number increased to 96% in 80-year-olds. Similarly, asymptomatic disc bulges appear in 30% of 20-year-olds and 84% of 80-year-olds. It’s clear that this is a normal age-related change, and not one undeniably correlated with pain.
And it’s not an isolated finding. Fifty percent of people over the age of 60 have tears in the rotator cuff (a group of muscles that help stabilize the shoulder) with no pain. Eighty-five percent of adults have knee arthritis that doesn’t cause pain. One-third of people with heel spurs on x-ray have no pain at all.
We’ll explore what is actually causing the pain, and what you can do about it, but for now this comforting thought can help: if there is a group of people who have worrisome findings on imaging but no pain, then you, too, can be a part of that group.
Hurt Does Not Equal Harm
Perhaps you’ve been given this discouraging news: your running days are over. Don’t squat anymore. Be careful; if it hurts, don’t do it. Rest is best.
But by now you should be thinking, if it’s possible to have degenerative joint disease and not have pain, doesn’t this mean there’s a way back to doing the things you love?
The answer, we now know, is a resounding yes. Not only is it possible to become active again, but there is a very real danger in not doing so. Avoidance of activity leads to deconditioning of muscles and joints, which need to be strong and functioning well to take on the demands of daily life. Muscles and joints that are reinforced through activity can undergo this stress without harm. Continuing to avoid the activity can lead to a system of muscles and joints that can’t withstand stress, which continues the vicious cycle of injury.
If muscles and joints need exercise to become stronger, but exercise hurts, what can be done? If passive treatments to reduce pain can help you get over the hump enough to perform the exercise well enough that it is tolerable, then we’ve met you halfway. We are chiropractors, after all, and pain is something we are good at dealing with. But even so, it is important to recognize that hurt does not always equal harm. The idea that pain is merely an alarm bell telling your brain that something in the body is damaged and needs rest is an old but outdated idea. The brain has top-down effects on pain, too. The brain can turn pain up or down. At our clinic, we are trained to help patients recognize when pain is a sign of injury (“red light” pain) or a warning signal for potential pain (“yellow light” pain). This in turn can help you have a positive experience with movement by confronting the fear of pain. Motion is lotion, movement is improvement.
Does This Mean It's All in My Head?
One of the major difficulties that practitioners have (the ones who are educated in pain science) is explaining to patients the brain science of pain in a simple, understandable way without making it sound like it’s all in your head. This is the last message that we want to convey. It can be helpful to destigmatize this idea by considering the spinal cord. Most people, if they were told that something was wrong with the spinal cord, wouldn’t feel the sense of shame that seems to upset many people when told something is wrong with their brain; yet the spinal cord is part of the central nervous system just like the brain and behaves in very similar ways. It and the brain can become more or less sensitive to the signals that could indicate pain. Pain just means your brain feels threatened by something from the environment. It can come from actual damage or potential damage. It can come from nerves that are irritated by tight muscles, joints that don’t move as well as they used to, thoughts, beliefs, and emotions about pain, or all of the above.
If this is confusing to you, imagine that you are on an old ship, out at sea, and you are in the crow’s nest. You are keeping a lookout and you see something off in the distance that looks like a ship. Pirates! A sense of dread ensues. But then, you take another look and think about it for a second, and now you aren’t sure. It’s hard to tell from this distance. Can you really see the telltale sign of the skull and crossbones flag waving threateningly in the wind? You decide it’s better to be safe than sorry and alert the captain. The captain comes out with his spyglass and takes a look. At this vantage point it’s still hard to see it outright, but the captain has much more experience than you do and the clues about its appearance tell him it’s not a pirate ship, and he reassures you.
But let’s say that in the past year there has been a surge of pirate activity in the area, and the captain recently had a close shave with a group of them. Do you think now the captain will be more cautious? Do you think now, in the uncertainty of the situation, he’s more inclined to raise the alarm for all hands on deck? Probably.
In this analogy, you are the spinal nerves traveling to the spinal cord, and the captain is the brain at the top of the spinal cord. The experiences you have, just like the experiences of the captain, can prime your brain to be more or less attuned to the signals coming from the rest of the body, and influence whether the brain feels threatened by them, which is what you experience as pain. Understanding that hurt doesn’t equal harm can help you confront the fear of pain and build not only a more resilient musculoskeletal system, but a more resilient nervous system as well.
And in case you’re wondering if we’re actually going to adjust you at this chiropractic clinic, yes, there is evidence that joint manipulation is helpful in dealing with the neurological effects of chronic pain by helping to stimulate the parts of the brain that help control pain. I like the way that Michael Maxwell, a chiropractor from Canada, said it the best: the adjustment can help patients “receive, filter, and accept pain.”
What Can You Do to Help Me?

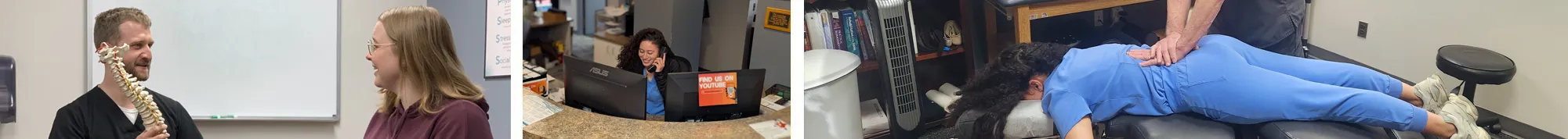
At Morrison Chiropractic, we know that some pain is a sign of serious harm. We are trained to examine you thoroughly to make sure your pain isn’t an emergency that needs medical intervention. Once serious pathology is ruled out, we guide you in a treatment plan that helps provide relief for symptoms and build a robust spine.
No two people have exactly the same treatment plan, because, as you’ve learned, pain and disability are not just an outcome of the diagnosis (though that can play a role), but also thoughts, beliefs, behaviors, experiences, and cultural context. During your treatment plan, we hope you remember that:
- Pain is an alarm that doesn’t necessarily indicate harm
- The brain can turn pain up or down
- Exercise can make your back strong
- Your body is made for movement!
OFFICE HOURS
Monday
7:00am - 7:00pm
Tuesday
7:00am - 7:00pm
Wednesday
7:00am - 7:00pm
Thursday
7:00am - 7:00pm
Friday
7:00am - 12:00pm
Saturday
7:30am - 12:00pm
Sunday
Closed
Morrison Chiropractic
2850 N Ridge Rd #107
Ellicott City, MD 21043