Tendinitis, Tendinosis, Tendinopathy - What’s in a name? What’s the most rational treatment in Ellicott City MD?

We frequently have patients who present at our Ellicott City MD chiropractic office with tendon pain. Tennis elbow, golfers’ elbow, shoulder tendinitis, hip “bursitis” or tendinitis, patella tendinitis, Achilles tendinitis. If they’ve seen their PCP or Orthopedist beforehand, they’ve been told they have “tendinitis” and offered NSAIDs (Ibuprofen, Naproxen sodium or others), a cortisone injection, and likely a stretching exercise handout.
The word "tendinitis" suggests the presence of inflammatory chemicals (cytokines) and thus the above prescription. Further research tells us that what is really occurring is degeneration of the tendon without the presence of inflammation, necessitating a new word: tendinosis. The focus was then on regenerative measures such as platelet-rich plasma injections, stem cell injections, and sclerosing injections. Outcomes were poor.
But wait, there’s more! The most comprehensive modern research comes from the Australian group, led by Jill Cook, Ph.D. (1). Their work suggests that there are three stages of disease (pathology) that occur in tendon pain and dysfunction. They are 1) reactive 2) dysrepair and 3) degenerative. Collectively known as tendinopathy. The even more complicated picture reveals, (surprise!) all three of these states can occur in the tendon at once!!
How does this affect treatment you ask? The documented presence of little to no inflammation calls the use of NSAIDs into question, perhaps of limited use at onset, but these interfere with the dysrepair/repair cycle and may in fact be contraindicated. Cortisone/steroid injections are potent anti-inflammatory agents. They may provide immediate relief, but research tells us they frequently impair long term outcome (2) and even weaken/damage tissue.
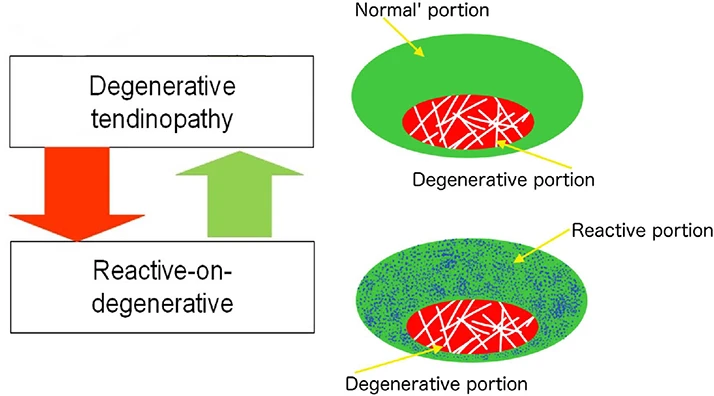
Schematic representation of ‘reactive-on-degenerative’ tendinopathy. A representation of the presentation on ultrasound tissue characterization is presented by Rudavsky and Cook.(4)
The drawing above shows the presence of all three phases of tendinopathy present in the same tendon, a common presentation. This can be visualized on ultrasound. Bad news- degenerative portion cannot be repaired. Good news- reactive portion can be restored and improved. Robust function without pain can be achieved! Kind of looks like a donut! You focus your treatment on the donut, not the hole. PRP, Stem cell, do not appear to address any of these stages (1).
What is the magic treatment? For pain we recommend avoidance of triggering activities initially (stop tennis, limit stairs, avoid sleeping on painful side at night), manual therapy or Graston® instrument-assisted soft tissue mobilization, Dry needling, topical analgesic, sport tape. Stretching is generally not recommended. This is the beginning of treatment. The real improvement happens with appropriate selection of just the right exercises, performed in a prescribed manner to precisely add load and stimulate repair and not overload the tissue! This requires expertise, diligence and patience. Along with this is evaluation of all the related structures that may increase load on the tendon to injurious levels. Poor spine mobility, ineffective “core”, weak gluteal muscles, tight hips, stiff ankles, unstable shoulder mechanics are some of these. Evaluation and improvement of these dysfunctions of your “kinetic chain” is your chiropractor’s role.
What follows is some sage advice adapted from my colleague Dino Papas, DC that he shares with his tendinopathy patients to help create realistic expectations and achieve long lasting benefit.
Tendinopathy Facts in Ellicott City MD:
1. Slow Cook This Like Good Barbecue: “low and slow”. 200 degrees for 12 hours to get that nice smoke flavor. Consistent daily loading of 10-15 reps over weeks to months is encouraged. We typically recommend 1 set of 10-15 reps done slowly 4-6x daily
2. Avoid excessive stretching. Stretching has been shown to increase end range pain tolerance but will decrease strength and functional performance and may actually compress the tendon and make the problem worse.
3. “How much pain should I tolerate?” Using 0-10 pain scale: 1,2,3,4 & "No more" ... 6, 7,8 & "I hate": Pain during loading should be tolerable 1-4/10 --- 6-8+/10 is too much load. Pay attention to the 5/10. If trending up from 5/10 then modify. If trending at 5/10 or down from 5/10 continue.
4. "Produce & No Worse": Loading tendinopathies can produce pain but later (minutes to hours later) the pain should return to baseline. This is important because many exercise prescriptions should not produce pain, but tendinopathies have a tendency to be different. Pain (tolerable pain) is highly likely with loading and loading is required for management and a successful outcome in many cases.
5. Watching Paint Dry: The paint will dry. It will just take time. The rehab isn't sexy. It's 1-2 exercises several times daily for months. If we assessed correctly, your tendinopathy will get better, it just will take time. Most protocols are 4-12 months long. Typically, functional improvement results begin at 2-3 months but we won’t' abandon the protocol until at least a 4 month trial.
7. Progressive Overload is Required to make the tendon "Bigger, Faster, Stronger and Harder to Kill": Start simple and progress. Isometrics --- Concentrics -- Eccentrics --- Functional Task Loading. Throughout this process your doctor may need to pump the breaks periodically or adjust and step on the gas depending on where you are in the process.
8. Treatment Plan: Requires several visits with manual therapy or other tools for pain control. Then emphasize progressive loading learned in office, performed at home. We "check"/re-evaluate baselines in office periodically for signs of progress.
9. Slow Healing Tendinopathies: Find out what's pumping the break.
Metabolic Concerns = Functional Medicine Work up- refer to Integrative Health Practices https://integrativehealthpractices.org/
Other medical specialty referrals may include Pain Management, Cognitive Behavioral Therapy.
Long Standing Tendinopathies that have improved but plateaued = Consider additional loading or rarely orthobiologic/regenerative medicine referral.
Contact our chiropractic team at Morrison Chiropractic for more information.
By Dr. Brian Morrison
- Cook JL, Rio E, Purdam CR, et al. Br J Sports Med 2016;50:1187–1191.
- Coombes BK, Bisset L, Vicenzino B. Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: a systematic review of randomised controlled trials. Lancet. 2010 Nov 20;376(9754):1751-67. doi: 10.1016/S0140-6736(10)61160-9. Epub 2010 Oct 21. PMID: 20970844.
- McAlindon TE, LaValley MP, Harvey WF, Price LL, Driban JB, Zhang M, Ward RJ. Effect of Intra-articular Triamcinolone vs Saline on Knee Cartilage Volume and Pain in Patients With Knee OsteoarthritisA Randomized Clinical Trial. JAMA. 2017;317(19):1967-1975.
- Rudavsky A, Cook J. Physiotherapy management of patellar tendinopathy ( jumper’sknee). J Physiother 2014;60:122–9.
OFFICE HOURS
Monday
7:00am - 7:00pm
Tuesday
7:00am - 7:00pm
Wednesday
7:00am - 7:00pm
Thursday
7:00am - 7:00pm
Friday
7:00am - 12:00pm
Saturday
7:30am - 12:00pm
Sunday
Closed
Morrison Chiropractic
2850 N Ridge Rd #107
Ellicott City, MD 21043